IMPROVING OUTCOMES FOR
Tear trough fillers
Ms Caroline Wilde and Professor Daniel Ezra discuss the ‘Three-Point Tangent Technique’
As healthcare professionals, we understand the impact that ageing can have on the delicate periorbital area. With advancing age, changes occur, such as the formation of the nasojugal fold or tear trough deformity medially and the palpebromalar groove laterally.1 These changes are often a result of volume loss in the midface, including loss of facial fat and descent of the malar fat pad. Additionally, the elongation of the orbital retaining ligament and orbital septum laxity contribute to the prominence of the orbital rim and exposure of the infraorbital fat pads. These factors, combined with the inelasticity and tethering effect of the lower lid retaining ligaments, lead to the formation of the tear trough deformity.
Tear trough fillers have gained immense popularity in addressing under-eye bags and hollowing, providing a quick and effective solution for many patients.2 However, the delicate and unforgiving nature of the tissues in the under-eye area poses challenges, including a greater propensity for visible swelling and lumps. Furthermore, the dense vascular supply in the periorbital area increases the risk of complications such as bruising, vascular occlusion, and retrobulbar haemorrhage. To minimise these risks and ensure optimal outcomes, a thorough understanding of periorbital anatomy is essential.
In our quest to enhance the outcomes of tear trough filler treatments beyond current standards, we have developed a revolutionary injection technique known as the Three-Point Tangent Technique. This technique utilises a blunt cannula to deliver filler along three linear tangents, tailored to each patient’s unique anatomy. By deconstructing the tear trough hollow into linear components, our goal is to minimise tissue trauma and achieve precise filler placement. Our recent publication in Plastic and Reconstructive Surgery Global Open includes the largest series to date of tear trough fillers, which not only validates the effectiveness and safety of this technique but also demonstrates better outcomes when compared to previous studies.3
Patient selection is crucial in tear trough filler treatments, and it is important to counsel patients regarding expected results and potential complications. Realistic expectations should be set, and patients should understand the small but real risk of vascular occlusion or retrobulbar haemorrhage, which can lead to vision loss. The ideal candidates for tear trough fillers are those with a defined hollow in the under-eye area. If patients have bags or bulges in the lower eyelid caused by fat herniation, blepharoplasty surgery should be discussed although filler can be used to disguise smaller bags. Patients must also be told that tear trough fillers do not address dark circles, and patients should be informed that fillers can improve shadows created by hollowing but cannot alter skin colour or reduce pigmentation.
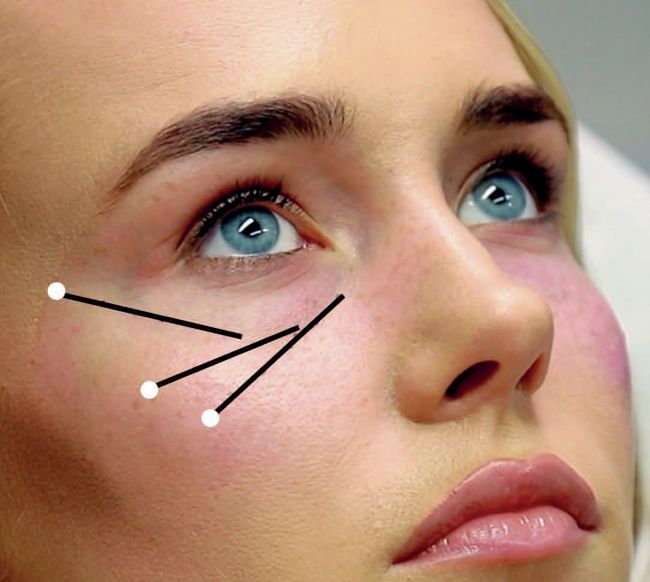
The
tear
trough
is
deconstructed
into
three
tangents.
The
entry
point
for
the
needle
is
demonstrated
by
a
white
circle
and
the
black
line
represents
the
planned
linear
deposition
of
the
filler.
The Three-Point Tangent Technique involves delivering filler along three tangents that correspond to the tear trough deformity’s anatomy. The arc of hollowing under the eye from the tear trough medially to the palpebromalar groove laterally should be divided into three linear segments.
The skin is stretched and punctured with a 25 gauge needle at the end of the linear tangent away from where the filler will be injected. A 25 gauge, 40mm blunt cannula is inserted in a suborbicularis plane. Small aliquots of filler are deposited while withdrawing the cannula, ensuring even distribution. Massage is performed to mould the filler and ensure its proper placement. This is repeated three times for each tangent. The presence of the orbicularis retaining ligament condensation may cause resistance during cannula insertion laterally, which can be overcome with controlled pressure. To avoid posterior filler injection, the cannula is always passed in the coronal plane. Following treatment, patients are advised not to wear makeup for 24 hours but can resume their normal activities the following day.
In our comprehensive study, we conducted a retrospective case review of 1,452 tear trough filler applications on 583 patients between 2016 and 2020. Our findings demonstrate positive outcomes and minimal complications associated with the Three-Point Tangent Technique. The majority of patients (82%) reported no complications after their initial treatment. For the remaining patients, complications were generally mild and temporary, including swelling (10%), bruising (4.3%), contour irregularities (4.6%), and the Tyndall effect (3.3%). Notably, one patient (0.17%) experienced a retrobulbar haemorrhage, which was promptly managed with an emergency canthotomy and cantholysis without any lasting visual compromise.
Our study also contained a data analysis to identify independent predictors of complications. We identified several key factors that significantly influenced the outcomes of tear trough filler treatments. The volume of filler injected emerged as a crucial factor in the occurrence of complications, particularly oedema (swelling) and contour irregularities. Our analysis revealed a clear association between injection volumes exceeding 0.3ml and the occurrence of oedema. This finding emphasises the importance of controlled dosages to achieve optimal outcomes.
Oedema emerged as the most common complication, affecting 10% of patients following their first filler injection. However, conservative measures successfully resolved oedema in 84% of cases. Furthermore, complete resolution was achieved within four weeks for half of the patients, irrespective of the volume of filler injected. This highlights the effectiveness of waiting four weeks for the resolution of oedema before considering intervention and supports patient decisions regarding the use of filler-dissolving injections.
Patients who had previously undergone filler dissolving were significantly more likely to require additional dissolving after subsequent re-injections. This highlights the importance of providing thorough counselling to patients regarding the potential need for further dissolving when addressing filler-related issues. It is crucial to educate patients that re-treatment with filler may lead to the recurrence of the same problems they initially presented with, necessitating additional dissolving. Factors such as constitutional patient characteristics can contribute to the development of oedema and contour irregularities. Therefore, special caution should be exercised when considering fillers in these patients, taking into account their medical history and potential predisposition to complications.
The Three-Point Tangent Technique offers significant advantages over traditional tear trough filler injection methods. By utilising a blunt cannula, tissue trauma is minimised, and the risk of complications is reduced. Precise and natural-looking filler placement is achieved by deconstructing the tear trough hollow into linear components. Placing the filler under the orbicularis oculi muscle ensures even distribution and prevents visible lumps or the Tyndall effect without increasing the risk of vascular occlusion. In addition, the conceptual deconstruction of the complex contours of the tear trough deformity into linear components provides a framework to approach this complex problem.
In conclusion, the Three-Point Tangent Technique represents a safe and effective method for rejuvenating the under-eye area. Our comprehensive study, which includes the largest number of tear trough filler applications, demonstrates the excellent outcomes and minimal complications associated with this innovative technique. By focusing on precise filler placement and reducing tissue trauma, this technique achieves optimal results while prioritising patient safety and satisfaction.
MS CAROLINE WILDE
Ms Caroline Wilde is an ophthalmic and oculoplastic surgeon, renowned for her expertise in blepharoplasty surgery, eyelid procedures, and advanced facial aesthetics. Her current research focuses upon improving outcomes in tear trough filler, blepharoplasty surgery and brow lifts. Patients can arrange appointments at her Harley Street Clinic.
PROFESSOR DANIEL EZRA
Mr Daniel Ezra specialises in all aspects of primary and revision blepharoplasty, cosmetic and reconstructive eyelid surgery, and lacrimal disease. All treatments offered by Mr Ezra are individually planned, from a range of options, to deliver the desired outside. Preoperative and postoperative care is provided by him personally in one of his London clinics.
REFERENCES
1.Ting M, Ezra DG. Unravelling the Complex Anatomy of the Tear Trough and Lower Eyelid Folds:A Review of Cadaveric Studies in the Literature. Journal of Craniofacial Surgery. 2022 Aug 10:10-97.
2. Morley AM, Malhotra R. Use of hyaluronic acid filler for tear-trough rejuvenation as an alternative to lower eyelid surgery. Ophthalmic Plastic & Reconstructive Surgery. 2011 Mar 1;27(2):69-73.
3. Wilde CL, Gupta A, Lee S, Ezra DG.Tear Trough Filler Using the Three-Point Tangent Technique: Lessons from 1452 Tear Trough Applications. Plastic and Reconstructive Surgery Global Open. 2023 Jun;11(6).