CLINICAL
Reversing dermal filler blindness
Dr Patrick Treacy summarises his key findings around reversing blindness caused by dermal filler

Blindness is a rare but serious complication that can occurwhen a dermal filler is injected into a blood vessel, blocking the flow of blood to the eye, and causing vision loss. The risk of blindness is higher when dermal fillers are injected into the glabella (between the eyebrows) and the nose area. This is a rare but serious complication of facial filler injection, and these complications date back decades and are long associated with facial aesthetic enhancement.1,2Even before hyaluronic acid (HA) was used as a dermal filler, injectable ‘collagen’, silicone, and autologous fat were also linked to similar occurrences. 3HA fillers revolutionised the procedure of facial enhancement because of the possibility of reversal of complications, such as visual loss, by using an enzyme called hyaluronidase, which breaks down the HA and allows the blood vessel to open again, restoring blood flow and hopefully preventing permanent damage to the eye. The supraorbital and retrobulbar methods are two proposed different approaches for treating dermal filler blindness.
SUPRAORBITAL VS RETROBULBAR
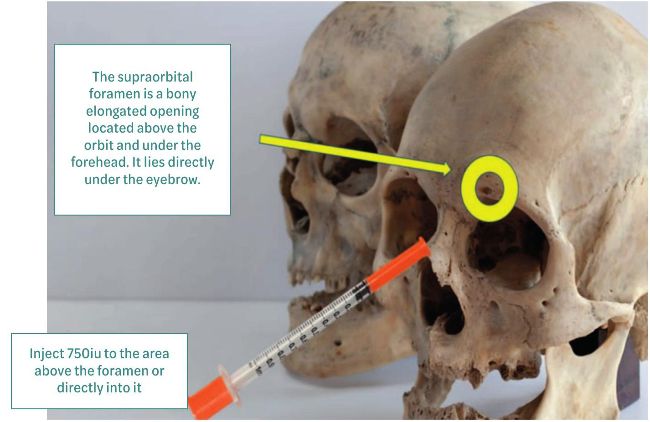
The supraorbital method involves injecting hyaluronidase into the supraorbital foramen, specifically into the supraorbital artery, which is located above the eyebrow. This method requires no special skills, is less invasive than the retrobulbar method and can be effective in cases where the blood vessel blockage is closer to the surface of the skin.
IMMEDIATE
• Local pallor
• 1500 U diluted in 6cc saline
• Needle 30 g ½
• Bolus subcutaneously + supraorbital
• Multiplex entries
• Massages
• Improves pallor

3000 units in supraorbital foramen
The retrobulbar method, on the other hand, involves injecting hyaluronidase under the globe of the eye, specifically into the retrobulbar space, which is located under and behind the eyeball. This method is more invasive than the supraorbital method but can be necessary in cases where the blood vessel blockage is deeper in the tissue. The idea of a retrobulbar hyaluronidase as rescue therapy was conceived back in 2013 by ophthalmologist Jean Carruthers and other members of an advisory board, after a flurry of cases of reported sudden onset blindness/visual loss during injection with HA fillers in Asia.4,5I had reservations about this method and expressed my opinion in an article published that year in Body Languagemagazine, proposing the supraorbital route instead. 6My main reason for suggesting this method was that the risks were high, and vision rescue was unlikely, as the central retinal artery, once inside the nerve where the embolus may be lodged, is covered with three layers of meninges and located very posteriorly in the retrobulbar space. Only 5mm or less of the ophthalmic artery was exposed in orbit that was not covered with dura. Hence, the hyaluronidase would have trouble reaching the embolus itself. The original article can still be found here. 7
Diagnosis of ophthalmology: “embolism of Ophthalmic Artery, grade 4, the most severe, blindness is irreversible after 4 hours”
FURTHER RESEARCH
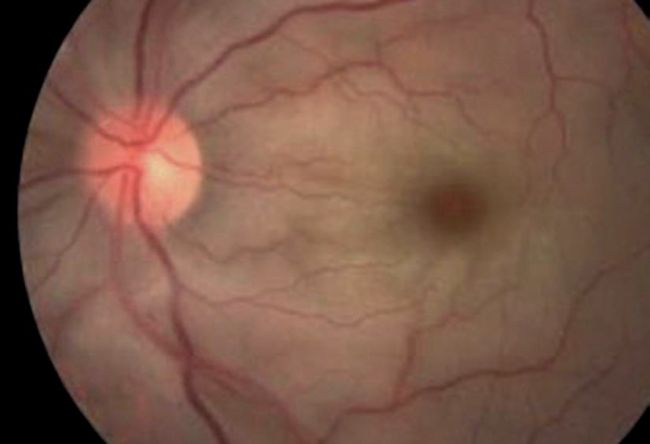
Retrobulbar hyaluronidase injection was advocated by several ophthalmic and plastic surgeons for many years as an emergency treatment, but never proved itself in terms of its efficacy. A paper by Guo-Zhang Zhu8suggested that retrobulbar hyaluronidase injection may not be an effective rescue treatment for vision loss caused by HA filler embolisation. However, it is important to note that this is a small study with only four patients and a low level of evidence, so further research is needed to confirm these findings. One patient with branch retinal artery occlusion (BRAO), one with posterior ischemic optic neuropathy (PION), one with ophthalmic artery occlusion, and one with both BRAO and PION were treated with one or two retrobulbar injections of 1500 or 3000 units hyaluronidase. No patients demonstrated substantial retinal artery recanalisation or vision acuity improvement after treatment. Another paper by Lei Pan and Hong XuGuo-Zhang Zhu8 noted that the severity of blindness caused by HA injection may be associated with the occlusion site. They concluded that conventional treatments, such as retrobulbar hyaluronidase injection, are insufficient to relieve visual impairment. Injecting as little as 0.08 ml of HA into the facial branch is enough to cause a central retinal artery embolism. Another paper by Surek 9falsely claimed that retrobulbar injection with hyaluronidase is the only known potential means of reversing this adverse event but correctly concludes positive outcomes remain anecdotal.
10 MINUTES LATER
• Pain right eye
• Homolateral headache
• Nausea
• Palpebral ptosis
DAY 14: WATCHING 20/25 +2
There is almost 100% vision
REFERENCES
1. Chesnut C, Restoration of visual loss with retrobulbar hyaluronidase. injection after hyaluronic acid filler. Dermatol Surg 2018;44:435–7.
2. Lazzeri D, Agostini T, Figus M, Nardi M, et al, Blindness following cosmetic injections of the face. Plast Reconstr Surg 2012;129: 995–1012.
3. Teimourian B, Blindness following fat injections. Plast Reconstr Surg 1988;82:361.
4. Kim EG, EOM TK, Kang SJ, Severe visual loss and cerebral infarction after injection of hyaluronic acid gel. J Craniofac Surg 2014;25:684–6.
5. Kim YJ, Sim SS, Song WK, Lee SY, et al, Ocular ischemia with hypotony after injection of hyaluronic acid gel. Ophthal Plast Reconstr Surg 2011;27:152–5.
6. Treacy P, Facing complications. Body Language 2015;77:20 6.
7. https://www.linkedin.com/pulse/dr-patrick-treacy-discusses-dermal-filler-how-deal-them-treacy/
8. Aesthet Surg J . 2017 Dec Efficacy of Retrobulbar Hyaluronidase Injection for Vision Loss Resulting from Hyaluronic Acid Filler Embolization Guo-Zhang Zhu , Zhong-Sheng Sun , Wen-Xiong Liao, Bing Cai, Chun-Lin Chen, Hui-Hui Zheng, Li Zeng, Sheng-Kang Luo
9. Aesthetic Plast Surg. 2019; 43(4): 1054–1060, Clinical observations and the anatomical basis of blindness after facial hyaluronic acid injection, Lei Zhang, Lei Pan, Hong Xu, Sheng Yan, Yi Sun, Woffles T. L. Wu, and Sufan Wu
10. Aesthetic Plast Surg 2019 Aug, Retrobulbar injection for hyaluronic acid gel filler-induced blindness: A review of efficacy and technique, Christopher C Surek, Sayf A Said, Julian D Perry, James E Zins
11. Dermatol Surg 2016 Apr, A rethink on hyaluronidase injection, intraarterial injection, and blindness: Is there another option for treatment of retinal artery embolism caused by intraarterial injection of hyaluronic acid? Greg J Goodman 1, Mike D Clague
CONCLUSIONS
In 2016, I read an article by Greg J Goodman and Mike D. Clague on treating a potential occlusive eye injury by using the supraorbital route.10They stated: “A female patient was being injected deeply in her temples and brow with HA when she noted a flashing sensation in her right eye and partial loss of vision. The practitioner then injected approximately 0.8 mL (300 units) of hyaluronidase twice in short succession into the area of the supratrochlear and supraorbital notches with the second injection bringing instant relief of visual symptoms and return of eyesight. Subsequent ophthalmic review and magnetic resonance imaging illustrated no retinal artery or product intracerebral event”. The presumed mechanism for this catastrophic event has been suggested to be the retrograde flow of the filler in the artery congesting the peripheral branch of the blood vessel pushing against the arterial pressure until the flow reaches past the section of the ophthalmic system where the retinal artery begins. Some other cases were reported from China during the lockdown at the St. Petersburg Multidisciplinary Aesthetic Medicine Congress on June 17-20. The most interesting development was a session by Dr Fernando Silikovich at IMCAS 2023, where he presented a case, he had reversed using the supraorbital method (images shown). Some fascinating work has been done by Ha Hong Nguyen, a plastic aesthetic surgeon at Viet Duc University Hospital, in Hanoi, Vietnam, who has reversed some cases of dermal filler-induced blindness by direct cannulation through the internal carotid arterial route. I am thankful to Dr Fernando Silikovich for recognising me as the first advocate of using the supraorbital method of treating dermal filler-induced blindness and strongly recommending its use formanyyears now.
DR PATRICK TREACY
Dr Patrick Treacy is the founder of the Ailesbury Clinic, Dublin. Recognised globally as a leading pioneer and expert in aesthetic medicine, he is currently President of the Royal Society of Medicine (London) Aesthetic Faculty and Chairman of the Irish Association of Cosmetic Doctors. He was recently made visiting Professor of Dermatology at Isra University in Pakistan and received an Honorary Fellowship in Cosmetic Surgery from the Australian College of Cosmetic Surgery and Medicine.