CLINICAL
PHOTODYNAMIC THERAPY
Dr Robin Stones and Jan Birch share their experiences treating acne and photodamaged skin with 2% 5-aminolevulinic acid-based photodynamic therapy
JAN BIRCH
Jan Birch has been a dermatology specialist for over 20 years. She left the NHS to work in clinical research, focusing on phototherapy and the development of LED Light sources to treat nonmelanoma skin cancers and other skin diseases. She is the managing director of Blemish Clinic and the director of a small clinical research company.
DR ROBIN STONES
A dermatology specialist with 30 years hospital experience, Dr Robin Stones is the clinical lead for a photodynamic therapy service treating non-melanoma skin cancer. With 20 years of experience in aesthetics, he is the medical director at SK;N clinic Wilmslow and was formerly the group medical director of Courthouse Clinics.
In the context of dermatology, conventional photodynamic therapy (PDT) utilises a topically applied, photosensitising drug – 5-aminolevulinic acid (5-ALA), or its methyl ester (MAL) – in conjunction with an activating light source, usually continuouswave red (633nm) LED. It is most commonly used to treat certain types of non-melanoma skin cancer. In this article, we will discuss the use of a new low-concentration 5-ALA, specifically for cosmetic indications.2
Light-only phototherapy creates a cascade of biochemical reactions, resulting in a physiological change within the target tissue, energising cellular function and stimulating collagen production, which improves skin laxity, while also reducing inflammation and erythema. The effects of light alone are known as ‘Photo biomodulation’.3
MECHANISM OF ACTION FOR PDT
PDT uses a light source of a specific intensity and wavelength to activate naturally occurring photosensitisers such as coproporphyrin III in Cutebacterium (C acnes) or to activate protoporphyrin lX (PPlX) following conversion of a topically applied photosensitising drug, such as 5-ALA or MAL.⁴
Conventional PDT for the treatment of non-melanoma skin cancer involves the application of topical 5-ALA or MAL to the target lesion, followed by a three-hour occluded incubation period, during which the photosensitiser undergoes enzymatic conversion into PPlX, which is then activated by a 633nm LED light, creating a photodynamic response.
Photoactivation and photobleaching of PPlX occur, generating oxidative stress and reactive oxygen species (ROS). This initiates inflammation and cytotoxicity, resulting in apoptosis and necrosis of abnormal cells.5
WHY USE RED LIGHT
• To generate a therapeutic effect, the spectral output of the light source should correspond to the excitation peaks of the photosensitiser
• PPIX has two important peaks, 404–420 nm in the blue (Soret band) and 635nm in the red wavelength region6
• The depth of light penetration into the skin increases with longer wavelengths
• Although blue light allows sufficient tissue penetration for the treatment of superficial AKs, red light penetrates much deeper structures, such as sebaceous glands
• In comparison trials, employing continuous wave light sources is more efficacious than pulsed light sources
• Light-emitting diodes are more effective as a light source compared with broad-spectrum white light.
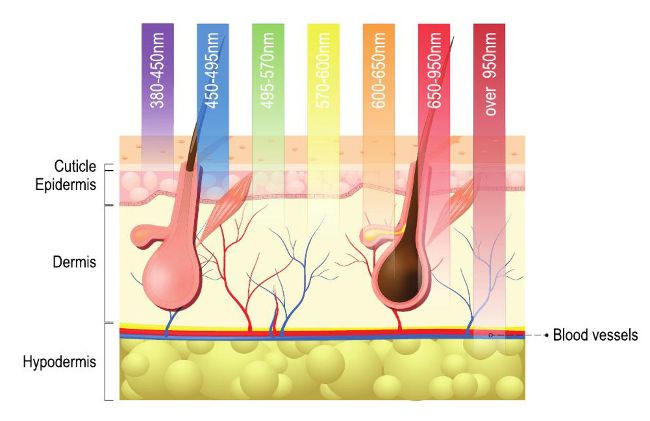
Wavelength-dependent penetration of blue, green, yellow, and red light in PDT. Arrows indicate the approximate 50% optical penetration depth in human skin.
5-ALA is a naturally occurring substance in the human body, being part of the pathway for the synthesis of haem in haemoglobin. It is a lipophilic molecule which is very well absorbed into the pilosebaceous unit. For this reason, there have been several trials using PDT to treat inflammatory acne. However, it is well documented that, when using conventional preparations of photosensitiser, patients can experience quite extreme reactions post-treatment, including pain, swelling, and phototoxicity, which limits the tolerability of PDT for cosmetic indications. The combination of prolonged incubation time of the drug to produce PPIX and light illumination times makes it less feasible for implementation in a private clinic.7
The recent introduction of GlycoALA, which employs glycosphere nanotechnology as a drugdelivery mechanism addresses many of the previously encountered limitations.
WHAT IS GLYCOALA?
GlycoALA uses Glycosphere nanotechnology1to deliver high concentrations of 5-ALA into the skin. Glycospheres are nanoparticles (200nm diameter) which can bind both hydrophilic and lipophilic actives. In the case of GlycoALA, the actives are hyaluronic acid and 2% 5-ALA. These actives are ionically bonded within the glycosphere and are only released in the target tissue (epidermis). 2
This enables the delivery of high concentrations of the actives in a shorter time, compared with conventional products, allowing lower concentrations of actives to be used and shorter incubation periods (40 – 60 minutes). When used in conjunction with an oxygen scrub to prepare the skin and an ultrasonic blade to exfoliate, the clinical outcomes are more predictable with fewer adverse effects. Three treatments at monthly intervals are recommended.
GlycoALA, which has a cosmetic license in the UK, is a very stable product with a long shelf life and does not require a cold chain in terms of transport and delivery. Each container is sufficient for six treatments (two patient courses of three treatments) making it very cost-effective.
GlycoALA not only has the benefits of treating larger surface areas of photodamage, and photoaging, but the ability to condition the skin and reduce the activity of sebaceous glands and, therefore, sebum production. The treatment reduces oiliness, comedones, inflammatory acne, and sebaceous hyperplasia.
GlycoALA PDT is an additional treatment option for medical practitioners which can be used in conjunction with other modalities. It also works in combination with selected skin care products and peels. It can be utilised with existing skin treatments to prepare the skin.
All Fitzpatrick skin phototypes are suitable for treatment with GlycoALA. However, the use of a tyrosinase inhibitor for darker skin types before treatment is essential.
Treatment protocols have now been optimised so patients can be prepared at the consent stage and the practitioner can be confident of the clinical outcome. Some patients experience greater photodynamic reactions, depending on their skin type and condition.
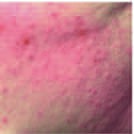
TYPICAL REACTIONS OF A GLYCOALA TREATMENT – MILD ACNE

Baseline

2 days post-treatment

30 days post-treatment
There are marked improvements in freckling, lentigo, and erythema
ANTERA 3D IMAGINING
REDUCTION IN PORE SIZE
Baseline
After GlycoALA
REDUCTION IN ERYTHEMA

Baseline
After GlycoALA
courtesy
of
Dr
George
Pouros

Baseline
2 weeks after 2nd treatment
CASE STUDY 1
A 14-year-old girl suffering from mild acne.
She had a mixture of inflammatory and noninflammatory lesions. Experiencing new lesions every day. She had two treatments of GlycoALA, four weeks apart.
CASE STUDY 2
Fitzpatrick 1V-V
This patient was treated with a botanical tyrosinase inhibitor two weeks prior to, and throughout treatment.
She had suffered from persistent acne since her early teens and had extremely oily skin. Having exhausted antibiotic treatment and over-the-counter (OTC) medication, she was referred for isotretinoin, but preferred an alternative treatment as she wanted to start a family in the near future.
She had four GlycoALA treatments four weeks apart and one further treatment 12 months later for active acne and her post-inflammatory hyperpigmentation.
CASE STUDY 3
A patient with extensive photodamage on his scalp and marked field changes
This 93-year-old gentleman was embarrassed to look in the mirror and wore a cap indoors to hide his scalp. He had surgical treatment for a previous BCC on his scalp, also regular cryotherapy for his actinic keratoses. He said he was unable to get furthertreatment from the NHS. He had scartissue from his previous surgery and extensive actinic damage. He felt GlycoALA treatment was ‘life-changing’.
The lesions were curetted prior to GlycoALA treatment. Three treatments were given four weeks apart, with no discomfort during the treatment.
40
mins
incubation
time

Pre-treatment

Post-treatment

Pre-treatment

2 weeks post treatment
CONCLUSION
GlycoALA PDT is a useful, non-ablative, painless treatment modality for cosmetic indications such as acne, photodamage, and sebaceous hyperplasia. It is suitable for all skin types and lifestyles and has very little downtime.
The development of glycosphere-encapsulated 5-ALA enables high concentrations of photosensitiser to be delivered rapidly into the target tissue resulting in shorter incubation times whilst maintaining predictable efficacy.
REFERENCES
1: Glycospheres: Delivery System Protection and Stability of Actives-ref. Gs-001/ October 31, 2014
2-The influence of UV exposure on 5-aminolevulinic acid-induced protoporphyrin IX production in skin. Von Beckeroth Meo , Photochem Photobiol, 2001 Dec; 74(6):825-
3 “ A Review of Molecular Evidence of Low Level Light Therapy” Graeme E Glass JPRAS Dec 27.2020 Vol (74) Pg 931-1160
4 -Photodynamic Therapy with ALA and blue light: Kathleen W. Judge, M.D. Medical Director Diplomate American Board of Dermatology and Dermatologic Surgery.
5 Guidelines for topical PDT: Colin Morten et al BrJ Dermatology 2002 April 146(4) 552-67
6 “Photodynamic Therapy:” A Review JS McCaughan Jr Drugs Aging (1999) July 15(1) 49-68
7 “Pain caused by Photodynamic Therapy of Skin Cancer” S. Grapengiesser et al Clin Exp Derm 2002 Sept, 27 (6)