INTIMATE REJUVENATION
MenoPAUSE
Aesthetic regenerative gynaecology and sexual medicine consultant Dr Nadia Yousri looks at turning back physical symptoms of the menopause
There are two definites in life: we will pay tax and we will die. Unfortunately, for women, there is a third: menopause. So, what is menopause and what choices do women have to combat the 50 known physical or mental symptoms they can suffer on their inevitable menopause journey?
Natural menopause is defined as one year after the women’s last period (the average age in the UK is 52.5 years). The time before is known as perimenopause, and, after, as the post-menopause. During this transition, there is a progressive decline in the level of the hormones oestrogen, progesterone and testosterone, and they eventually stop being produced altogether. The traditional standard in the treatment of menopause is Hormone Replacement Therapy (HRT), which replaces the loss of these hormones, alleviating the known menopausal symptoms.
Currently, NHS England is working with the government to implement longer prescribing cycles, in line with National Institute for Health and Care Excellence (NICE) guidelines, so women receive fewer prescriptions, reducing the need to pay frequent prescription charges. The government has asked NHS England to review current practices and the barriers to implementing NICE guidelines. This could mean women would only have to pay one charge for up to a 12-month supply of HRT, saving up to £205 per year as a result. To further improve access to HRT prescriptions, the government has also committed to investigating combining two hormone treatments into one prescription, which affects approximately 10% of women accessing HRT.
However, many women won’t or can’t take HRT due to personal or medical reasons, or because of historical HRT ‘scare mongering’. For example, 75% of women with breast cancer have a positive oestrogen receptor and need to be on anti-oestrogen medication like tamoxifen or an equivalent drug to reduce the recurrence which can cause early menopause.
Intimate female area rejuvenation is not only beneficial for women who suffer a lack of oestrogen during natural or surgical menopause or to combat the negative effects of cancer treatments, but also after pregnancy or weight loss. With ageing and a lack of oestrogen, there are major changes in the female intimate area, medically called vulvar-vaginal atrophy or genito urinary syndrome(GUS).
As a gynaecologist, I see ladies seeking treatment for gynaecological problems that are directly related to GUS characterised by atrophic changes, progressive loss of connective tissue support and pelvic floor relaxation. The most common symptoms are asymmetry, flattening or sagging of the labia majora, urinary discomfort and leakage, poor vaginal lubrication, burning and itching, loss of confidence regarding their femininity, sexual embarrassment and discomfort doing exercise. Loss of vaginal wall tone and weakness in the muscle controlling the anus can lead to faecal leakage. If not treated, more progressive sagging of the tissues occurs resulting in various degrees of prolapsing tissues.
To treat GUS conditions, conventional options were limited to conservative measures like Kegel exercises or the use of HRT, versus surgical options (surgical vaginoplasty or urine tube support operations). However, each option has its limitation or risks and is not suitable for everyone.
Surgery is effective but invasive, expensive and has inherent risks or complications besides long recovery time. Non-surgical procedures are increasingly more popular among patients, being non-invasive, requiring no or minimal analgesia, and with no downtime, hence gaining the reputation of lunchtime procedures. In the hands of experienced doctors, successful results can be achieved without complications.
The new medical subspecialty called aesthetic regenerative gynaecology offers both surgical and non-surgical approaches to reverse the manifestations of ageing-induced vulvovaginal atrophy and tissue laxity in the intimate female area, resulting changes in appearance and loss of lubricating functions in the area.
There are several non-invasive monotherapies to treat the physical symptoms and the changes in the intimate female area, such as HA fillers, Platelet-Rich-Plasma (PRP) and energy-based devices and topical intimate lotions and creams.
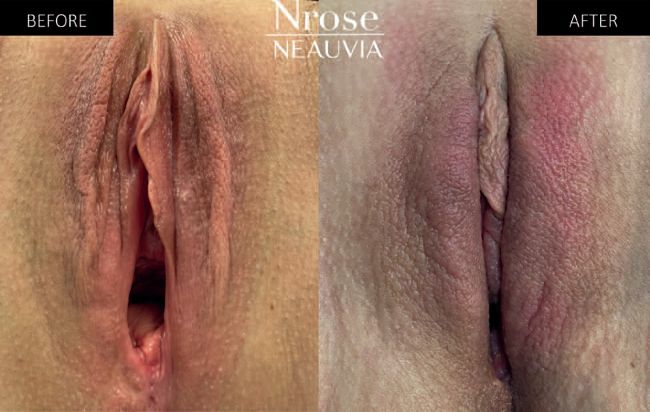
Neauvia has introduced Nrose, a clinical, evidenced-based, non-surgical, non-hormonal holistic protocol to treat genitourinary syndrome synergistically in sequence of four treatments over 12 days. It combines three monotherapies to optimise function. Nrose allows us to combine dermal fillers (intradermally) and an energy-based device (transdermally) in one treatment session, which is not only revolutionary, it saves time for the practitioner and patient and can also have an impact on cost per treatment.
The Nrose protocol is based on Smart Combination Therapy (SCT) which entails injecting Intense Rose, an HA-PEG intimate ‘heat-resistant’ filler, to restore and correct vulvar volume, shape, and rehydrate the skin and mucosa. It also strengthens the protective role of the labia majora and improves the aesthetic appearance of the vulvar-vaginal area. Together with Sectum, a bipolar radiofrequency device to tone, improve and tighten the vulvar tissue to give it a more youthful appearance. The treatment reconstructs the collagen and elastin, improves the blood flow, and increases the moisturiser in the vaginal canal in the first treatment session. This is followed by three more treatment sessions of Sectum and a twice-daily topical application called Rejuvenation Rose Gel serum, containing patented fractional hyaluronic acid and growth factors to complete the treatments.
Post-Nrose treatment, there is an immediate restoration of the protective role and the aesthetic appearance of the labia majora, supported by a 100% patient satisfaction rate and a signification increase of elastin and collagen fibres in the vulvar skin and the vaginal wall supported by the 20172 Intense Rose Study and the 20223 Nrose Protocol study.
REFERENCES
1. More support for women experiencing menopause: gov.uk/government/news/more-support-for-women-experiencing-the-menopause
2. A new hyaluronic acid polymer in the augmentation and restoration of labia majora. N Zerbinati, R GHaddad , A Bader et al. J Biol Regul Homeost Agents, 2017;31(2 Suppl. 2):153-161.
3. Hyaluronic Acid and Radiofrequency in Patients with Urogenital Atrophy and Vaginal Laxity Piotr Kolczewski 1, Mirosław Parafiniuk 2, Piotr Zawodny 3, Rashad Haddad 4, Agnieszka Nalewczyńska 5, Agnieszka Kinga Kolasa 6, Barbara Wiszniewska 6, Sophie Menkes 7, Alexander Bader 8, Giorgio Stabile 9, Nicola Zerbinati 10 Pharmaceuticals (Basel) 2022 Dec 16;15(12):1571. doi: 10.3390/ ph15121571.
DR NADIA YOUSRI
Dr Nadia Yousri is a fellow of the Royal College of Obstetricians and Gynaecologists in London, an OB&GY surgeon, and aesthetic regenerative gynaecology and sexual medicine consultant. She is triple board-certified in OB&GY and has been working in a top NHS university hospital for 22 years, as well as in her private practice in Harley Street, London. drnyaesthetics.com