CLINICAL
Metabolic syndrome and the skin
In our follow-up to last month’s article on understanding metabolic syndrome, Balsam Alabassi explores how it impacts skin and what you can do about it
There is increasing evidence to suggest a strong association between certain dermatological diseases and metabolic syndrome
Last month, we discussed the pathology of metabolic syndrome. Caused by a combination of diabetes, hypertension and obesity, the condition is not only dangerous to patients’ overall health, but can impact their skin too. Here we will explore commonly associated conditions while detailing how aesthetic practitioners can support affected patients.
RESULTING SKIN CONDITIONS
There is increasing evidence to suggest a strong association between certain dermatological diseases and metabolic syndrome.1Some of which include:
Psoriasis: defined as a multi-system inflammatory disorder of the skin, where the prevalence of metabolic syndrome is significantly higher in psoriatic patients than in unaffected individuals.2
Notably, research has suggested that patients with a higher Psoriasis Area Severity Index (PASI) score are more likely to develop metabolic syndrome.3In addition, psoriatic patients with metabolic syndrome have a longer disease duration compared to those absent from the disease. 4
It is interesting to note that treatment of psoriasis seems to exert a beneficial effect on the treatment outcome of related vascular diseases. This is seen in relation to the application of methotrexate therapy, which has been found to reduce the risk of major cardiovascular events in patients with psoriasis, psoriatic arthritis and rheumatoid arthritis compared to untreated control patients.5
Radtke et al. published an algorithm for psoriatic patients’ follow-up and recommended that metabolic syndrome screening be conducted every six months for patients with severe psoriasis and annually for mild cases of the disease. Furthermore, these patients should be advised to make lifestyle changes.6
Androgenetic alopecia: a benign disease and the most common type of hair loss. It is characterised by hereditary baldness, whereby the transformation of large terminal follicles to miniature ones is triggered by binding of dihydrotestosterone
(DHT) to androgenic receptors in hair follicles of the scalp. Genetic factors and family history may highlight the association between androgenetic alopecia and cardiovascular disease.5
Studies indicate that androgenetic alopecia in both males and females may be linked to increased obesity, hyperinsulinaemia and hyperaldosteronism. Elevated insulin levels may lead to vasoconstriction and reduced nutritional supply, further contributing to the effect of DHT on the miniaturisation of the hair follicles.7
On the other hand, hyperaldosteronism contributes to increased blood pressure and stimulates hair receptors to favour the progression of alopecia. Elevated free androgen levels and oxidative stress as a result of metabolic syndrome may worsen the disease.
What’s more, microinflammation in the hair follicles may also be a contributing factor.7
Acanthosis nigricans: a benign skin disease where hyperinsulinaemia interacts with epidermal keratinocytes, leading to the formation of the disease in frictional areas of the body.7It causes darkened, thickened patches in the armpits, neck and groin, which appear velvety in texture.
In a study conducted in an urban population of Sri Lanka, it was discovered that acanthosis nigricans was found to be more common among those with metabolic syndrome, irrespective of gender. In addition, a US study also found that 49% of fifth-grade children with acanthosis nigricans fulfilled criteria for metabolic syndrome.5
Skin tags: research has suggested that there may be a correlation between skin tags and insulin resistance. Some studies found more tissue leptin in skin tags than normal skin.5
Atopic dermatitis: an inflammatory skin condition with a systemic link has also been linked to metabolic syndrome. The relationship between atopic dermatitis and metabolic syndrome is being studied in a similar way to that of psoriasis, particularly as both skin conditions can co-exist.8
Hirsutism: along with irregular menstrual cycle, this is a feature of polycystic ovarian syndrome (PCO), where insulin resistance plays an integral role. PCO patients have a higher risk of metabolic and cardiovascular complications. Regular check-ups to rule out underlying factors should be the standard approach in all women with hirsutism. This is because the most common underlying cause of hirsutism in women of all ages is PCO.7
In a randomised trial, Rezvanian et al. demonstrated that adding metformin to intense pulsed light laser (IPL) significantly improves the hirsutism score compared to laser alone. They concluded that the treatment of underlying metabolic syndrome and the introduction of a more effective insulin sensitivity in women with hirsutism is a beneficial therapeutic approach.9
Hidradenitis suppurativa: also known as acne inversa, this is a chronic inflammatory disorder of the hair follicles. It is a painful condition and can present as recurrent nodules, abscesses and sinus tracts. It affects the armpits, anogenital and infra-mammary areas with rich apocrine glands.5Data has shown a positive link between the two conditions. 10
Atopic dermatitis: a chronic inflammation-related pruritic skin disease associated with metabolic syndrome. A meta-analysis of 30 studies has shown that central obese or overweight patients have a higher rate of atopic dermatitis compared with patients of normal weight.11
Acne vulgaris: an inflammatory disorder of the pilosebaceous gland affecting many adolescents and young adults. A study conducted by Nagpal et al. compared the metabolic conditions in 100 male acne patients and 100 male controls. Their findings suggested that the prevalence of metabolic syndrome tends to be higher in acne patients (17%) compared with controls (9%) (p = 0.09) and also that prevalence of insulin resistance is significantly higher in acne patients (22%) than controls (11%) (p = 0.03).12
Rosacea: a chronic skin disease with multifactorial causes and triggers defined by microcirculation abnormality and pilosebaceous disease of the skin.7Asurvey by Akin Belli et al. illustrated a correlation between rosacea and cardiovascular syndrome where the rate of insulin resistance in rosacea patients was higher than those in a control group.
In addition, dyslipidaemia and high-fasting glucose were also present in rosacea patients.13More research is needed to determine absolutes.
Lichen Planus: a chronic disease affecting the skin, mucous membranes, and appendages. Dyslipidaemia has been found to be significantly associated with Lichen Planus. In addition, there is also an increased prevalence of diabetes and carbohydrate intolerance that has been observed in patients with Lichen Planus.14
Systemic Lupus Erythematous (SLE): the prevalence of metabolic syndrome in patients with this condition varies between 17 to 40%. Studies have shown that premature atherosclerosis has been identified as an important cause of mortality in SLE patients, leading to a five to eight-fold increased risk of developing ischemic heart disease as compared to controls.5
Skin Cancer: some studies have shown metabolic syndrome is implicated in certain melanomas. However, more research is needed to establish findings.5
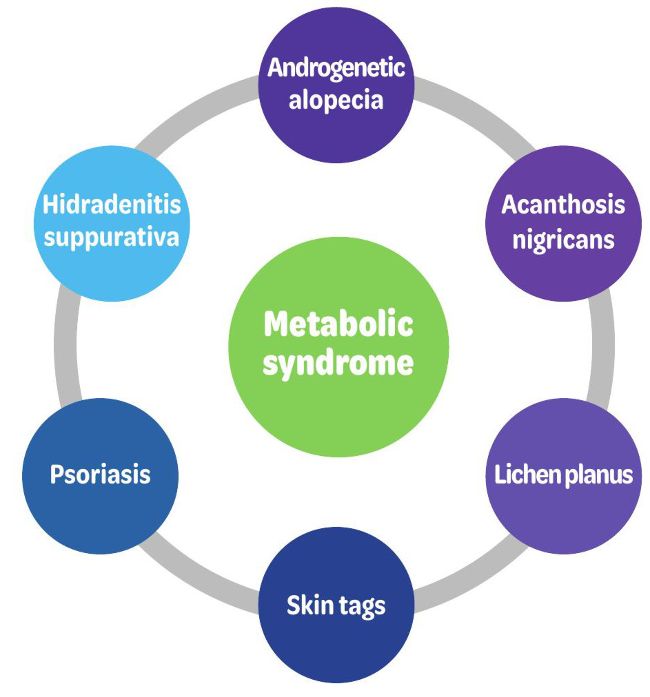
Figure 3: common cutaneous diseases associated with metabolic syndrome
CURRENT AND FUTURE THERAPIES
One formula does not fit all. Therefore, a multidisciplinary approach is needed for the diagnosis and treatment of metabolic syndrome, with a focus on the disease and its existing and potential co-morbidities.
Diet and exercise
Modification in nutrition and lifestyle play an important role in treatment.
This can be achieved through the application of the ‘plate method’ to relieve the strain on the pancreas by reducing the load and the rate that the pancreas needs to produce insulin through a review of carbohydrate intake and proportions.15
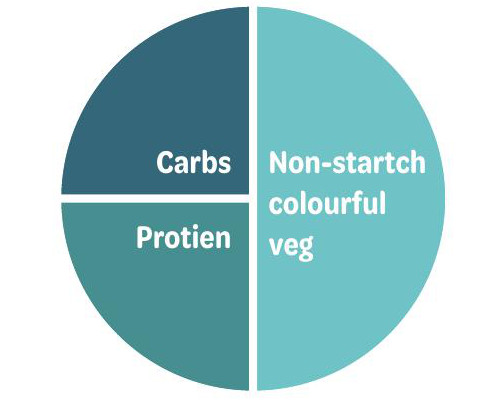
Figure 4: The plate method, a healthy split of nutritional content on a plate to manage insulin resistance.15
Moderate exercise can increase glucose uptake by approximately 40%. A 15-minute walk after a meal can have a huge impact on glucose levels. In essence, when insulin works well, the pancreas doesn’t need to produce quite as much of it.16
Pharmacological interventions
Weight loss management programmes through the application of GLP1 receptor agonists were originally developed for the treatment of diabetes.
Incorporating this with clinical patient selection is an effective option to manage glucose levels. It is worth noting that the application of GLP1 therapy should also be used in combination with a low carbohydrate and a low GI diet.17
Currently, the only licensed GPL1 receptor agonist for weight loss is Liraglutide, available under the trade name of Saxenda. Semaglutide, which is also GPL1 receptor agonist used for the management of diabetes, is currently prescribed off licence as Ozempic. This has been recommended by NICE in the UK and should be available under the brand Wegovy soon.18
Non-pharmacological interventions
There are a number of aesthetic interventions that manage a majority of cutaneous manifestations of metabolic syndrome. This includes the application of energy-based devices, one of which is LightPod Neo®, Aerolase.
The device features a novel 650-microsecond 1064-nm Nd: YAG laser and has received FDA approval for the treatment of psoriasis.19
The need to treat diversity is paramount where management of skin concerns for skin of colour is rapidly growing. Needless to say, this comes with challenges.
The LightPod Neo®, Aerolase, delivers energy in a collimated beam to administer treatments as stand-alone or in combination with other therapies. In my experience, the 650-microsecond can successfully and safely treat skin of colour, addressing a number of skin diseases linked to metabolic syndrome, as well as providing overall skin rejuvenation. What makes this device favourable is that the 650 microseconds are below the thermal relaxation time of the skin tissue. This, in turn, gives the skin time to cool itself between pulses, thereby confining the heat in the selectively absorbed target, leading to higher clinical efficacy and safety of the surrounding skin, sparing the patient from pain and downtime.20
Gut microbiome
The use of faecal microbiota transplants for metabolic syndrome and obesity are a proposed therapy that is being considered, with clinical trials in progress.21
Functional medicine
This is a rapidly growing field that focuses on the intricate causes of insulin resistance, using various diagnostic tools and tests to determine the most suitable treatment option.
SUMMARY
As discussed, there is a strong connection between metabolic syndrome and multiple skin diseases.
More research is needed to establish the link, however, current evidence does support the role of insulin resistance and chronic inflammation as major contributing factors.
While aesthetic modalities can manage skin manifestations as a consequence of metabolic syndrome, it is vital to treat the cause of the disease and advocate for the patient’s right to feel and look beautiful by providing a complete care solution for their skin health.
It is important to note that a patient’s psychological well-being is intimately related to the success or failure of managing metabolic syndrome and its effects. A multidisciplinary approach, focusing on the disease as well as its existing and potential co-morbidities, is therefore paramount.
REFERENCES
1. Hu, Y., Zhu, Y., Lian, N., Chen, M., Bartke, A. and Yuan, R., 2019. Metabolic Syndrome and Skin Diseases. Frontiers in Endocrinology, 10.
2. Qiao, J., Jia, Q. and Jin, H., 2020. Association between metabolic syndrome and psoriasis: a meta-analysis of observational studies with non-psoriasis control groups. Archives of Medical Science.
3. Boehncke, W. and Boehncke, S., 2014. More than skin-deep: the many dimensions of the psoriatic disease. Swiss Medical Weekly.
4. Cohen, A., Sherf, M., Vidavsky, L., Vardy, D., Shapiro, J. and Meyerovitch, J., 2008. Association between Psoriasis and the Metabolic Syndrome. Dermatology, 216(2), pp.152-155.
5. Padhi, T. and Garima, 2013. Metabolic syndrome and skin:
Psoriasis and beyond. Indian Journal of Dermatology, [online] 58(4), p.299. Available at: <https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC3726879/> [Accessed 7 April 2022].
6. Radtke, M., Mrowietz, U., Feuerhahn, J., Härter, M., von Kiedrowski, R., Nast, A., Reich, K., Strömer, K., Wohlrab, J. and Augustin, M., 2015. Early detection of comorbidity in psoriasis: recommendations of the National Conference on Healthcare in Psoriasis. JDDG: Journal der Deutschen Dermatologischen Gesellschaft, 13(7), pp.674-689.
7. Adibi, N. and Robati, R., 2021. Skin and metabolic syndrome: A review of the possible associations. Journal of Research in Medical Sciences, 26(1), p.16.
8. Stefanadi, E., Dimitrakakis, G., Antoniou, C., Challoumas, D., Punjabi, N., Dimitrakaki, I., Punjabi, S. and Stefanadis, C., 2018.
Metabolic syndrome and the skin: a more than superficial association. Reviewing the association between skin diseases and metabolic syndrome and a clinical decision algorithm for high-risk patients. Diabetology & Metabolic Syndrome, 10(1).
9. Rezvanian, H., Adibi, N., Siavash, M., Kachuei, A., Shojaee-Moradie, F. and Asilian, A., 2008. Increased Insulin Sensitivity by Metformin Enhances Intense-Pulsed-Light-Assisted Hair Removal in Patients with Polycystic Ovary Syndrome. Dermatology, 218(3), pp.231-236.
10. Gold, D., Reeder, V., Mahan, M. and Hamzavi, I., 2014. The prevalence of metabolic syndrome in patients with hidradenitis suppurativa. Journal of the American Academy of Dermatology, 70(4), pp.699-703.
11. Zhang, A. and Silverberg, J., 2015. Association of atopic dermatitis with being overweight and obese: A systematic review and metaanalysis. Journal of the American Academy of Dermatology, 72(4), pp.606-616.e4.
12. Nagpal, M., De, D., Handa, S., Pal, A. and Sachdeva, N., 2016. Insulin Resistance and Metabolic Syndrome in Young Men With Acne. JAMA Dermatology, 152(4), p.399.
13. Akin Belli, A., Ozbas Gok, S., Akbaba, G., Etgu, F. and Dogan, G., 2016. The relationship between rosacea and insulin resistance and metabolic syndrome. European Journal of Dermatology, 26(3), pp.260-264.
14. Fatima, F., Das, A., Kumar, P. and Datta, D., 2021. Skin and metabolic syndrome: An evidence-based, comprehensive review. [online] E-ijd.org. Available at: <https://www.e-ijd.org/ article.asp?issn=0019-5154;year=2021;volume=66;issue=3;spag e=302;epage=307;aulast=Fatima> [Accessed 7 April 2022]. 15. Salvi, R. and Abderrahmani, A., 2014. Decompensation ofβ-Cells in Diabetes: When Pancreaticβ-Cells Are on ICE(R). Journal of Diabetes Research, 2014, pp.1-7.
16. DUBÉ, J., ALLISON, K., ROUSSON, V., GOODPASTER, B. and AMATI, F., 2012. Exercise Dose and Insulin Sensitivity. Medicine & Science in Sports & Exercise, 44(5), pp.793-799
17. le Roux et al., 2017. Three years of Liraglutide versus placebo for type 2 diabetes risk reduction and weight management in individuals with prediabetes: a randomised, double-blind trial. The Lancet, 389(10077), pp.1399-1409. DOI:https://doi. org/10.1016/S0140-6736(17)30069-7.
18. NICE, NICE recommends new drug for people living with obesity https://www.nice.org.uk/news/article/nice-recommends-newdrug-for-people-living-with-obesity
19. Nestor, M., Fischer, D. and Arnold, D., 2020. Randomised, Investigator-Blinded Study to Compare the Efficacy and Tolerance of a 650-microsecond, 1064-nm YAG Laser to a 308- nm Excimer Laser for the Treatment of Mild to Moderate Psoriasis Vulgaris. Journal of Drugs in Dermatology, 19(2), pp.176-183.
20. Kesty, K. and Goldberg, D., 2020. 650 usec 1064nm Nd:YAG laser treatment of acne: A double blind, randomised control study. Journal of Cosmetic Dermatology, 19(9), pp.2295-2300.
21. Marotz, C. A., & Zarrinpar, A., 2016. Treating Obesity and Metabolic Syndrome with Fecal Microbiota Transplantation. The Yale journal of biology and medicine, 89(3), 383–388.