SKIN CANCER
Sun savvy
In honour of Sun Awareness Week last month, consultant dermatologist and author of The Skincare Bible, Dr Anjali Mahto, shares her guide to skin cancer
Dermatologists like to talk about skin cancer. A lot. It is one area of skin health that we do not want to ignore or miss. Rates of skin cancer in the UK have been rising significantly since the 1970s, and its incidence is thought to have increased as much as 360 per cent during this time.
Why is this? Since the 1970s, we have seen an increase in the accessibility of foreign travel and budget holidays in the sun. The desire to be tanned has become popular, and tanning bed usage more prevalent.
Combine this with the thinning ozone layer in parts of the world, and you can see how the problem has developed. Limiting ultraviolet light exposure remains the most important preventable factor in skin cancer.
There are three main types of skin cancer: melanoma, basal cell carcinoma and squamous cell carcinoma.
MELANOMA
Melanoma is the fifth most common cancer in the UK. It develops from the pigmentproducing cells in the skin, known as melanocytes. Melanoma can develop as a new mole on the skin (the majority) or within a pre-existing mole.
Ultraviolet light from the sun or artificial tanning beds is the single biggest culprit. Other risk factors include fair skin, multiple sunburns, a family history of melanoma in close relatives, conditions that cause a weakened immune system and the presence of lots of moles.
The reason we worry about melanoma is its ability to spread to other organs or ‘metastasise’
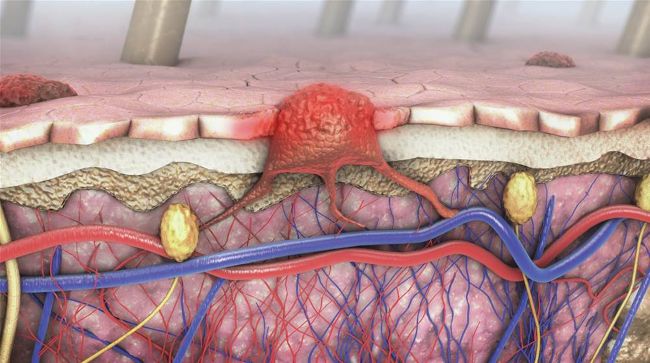
3d illustration of a cross-section of a diseased skin with melanoma
The reason we worry about melanoma is its ability to spread to other organs or ‘metastasise’. Melanoma has the potential to spread to the liver, lungs, bone and brain, where it can potentially be fatal. The good news is that most melanomas are picked up at an early stage, well before this happens.
There is no national screening programme in the UK for melanoma. The best chance of picking up a melanoma early is to know the signs and when to seek medical attention. I can’t stress enough how vital this is. For those who have private healthcare, many choose to have annual mole checks performed by a dermatologist as part of their preventative health screening.
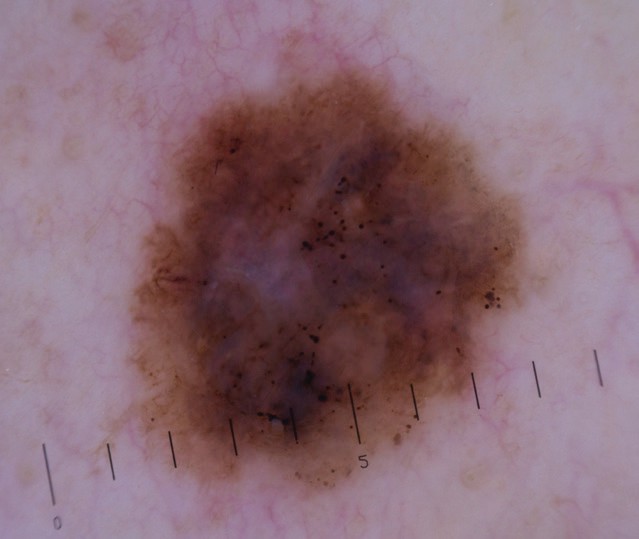
Dermatoscopic picture of melanoma - amalignant tumor from a mole
Educating your patients is key in bringing down rates of melanoma. The skin is a visual organ, and any surface changes should, in theory, be easier to pick up than disease in some other organ, which would require an internal scan.
EASY AS ABCDE
The acronym ABCDE is used most commonly as a tool for evaluating moles. If a mole shows any of these features, it warrants review by a dermatologist.
• Asymmetry: One half of the mole is different from the other.
• Border: The mole’s edge is irregular, scalloped or poorly defined.
• Colour: There is an uneven colour or variable colours within the mole.
• Diameter: The mole is bigger than 6mm in size.
• Evolving: The mole is changing in its size, shape or colour.
Other signs to look out for include any new moles or a mole that looks significantly different from the others (known as the ‘ugly duckling’ sign). The most common site for developing a melanoma in a male is the back, and in a female, the legs.
The tricky thing is that not all changing moles are indicative of skin cancer, and actually, most moles are harmless. It can be normal for moles to change in number and appearance; some can also disappear over time. Hormonal changes during puberty and pregnancy can cause moles to increase in number and become darker.
Most dermatologists recommend patients examine their skin themselves on a monthly basis. The ideal time is probably after a bath or shower in a well-lit room with the aid of a full-length mirror. Develop a system (e.g. from head to toe), first examining the front and then the back, to ensure no section of the body is missed. It can be helpful to get a trusted person to look at their back and other hard-to-examine areas. Take care not to forget sites like the buttocks, genital area, palms and soles. Some people find taking photographs once a year a good way to have a record of their skin. The first few months will purely be an exercise in getting used to where moles and blemishes are and what is normal for their skin. This becomes easier over time, although it can be challenging for those with many moles.
If someone has any concerns regarding a mole which is changing and you are not qualified to assess it yourself, make sure you refer them or encourage them to seek medical attention. They should visit their GP, who will either reassure them or refer them to a dermatologist, either on the NHS or privately. There are, therefore, multiple routes for seeking help depending on urgency and budget.
When a patient comes to see me, I usually carry out a total body skin examination with the aid of a dermatoscope. This is essentially a magnifying light, which allows us to see the details of the mole much more clearly to make an assessment. If there is any concern, the worrying mole is removed under local anaesthetic and sent to the lab for analysis, which will check for cancer. The mole removal is a quick procedure that takes twenty to thirty minutes and usually involves stitches to close the wound.
The majority of people who have a melanoma removed will have no further problems. However, this does rely on the melanoma being removed at an early stage. The bottom line remains that the earlier the melanoma is caught, the better the survival rate.

Different types of moles
HIGH STREET MOLE CLINICS
I’d advise caution when considering mole clinics. I often see patients that have previously been to such private clinics and learned that, frighteningly, many of these clinics do not have an in-house dermatologist and simply use a computerised machine to decide if a mole is worrying or not. If the machine flags the mole as a problem, they are then advised to see a dermatologist elsewhere.
From my point of view, there are a few issues with this, all of which I have seen first-hand:
• The technology is not sufficiently sophisticated at present to make a machine that is more reliable than a dermatologist.
• The machine is not able to look at the body as a whole and put what is seen into context. For example, my moles may all look slightly odd, but they are all the ‘same odd’; therefore, that may simply be normal for me. The machine is unable to use that human context.
• There are many situations where they might be told they have an ‘abnormal’ mole by machine mapping and then find out there is no in-house dermatologist to look at it or remove it. This generates a great deal of anxiety while they then have to find another clinic with a dermatologist.
• On several occasions, I have seen a supposed ‘abnormal’ mole that is actually harmless that has been removed and resulted in an unnecessary procedure and a scar. My advice would be to always get the mole reviewed by a dermatologist if there is a concern and cut out these middle steps.
• Even worse, in some of these clinics, a doctor without proper dermatological training will remove a mole purely because the machine flagged it, even though an inspection from a dermatologist would have indicated there was no need for concern, let alone surgery. Personal experience shows that this occurs surprisingly often.
NON-MELANOMA SKIN CANCER
There are two main types of non-melanoma skin cancer: basal cell and squamous cell carcinoma. Ultraviolet light, usually from the sun, is yet again the most common cause of their development. These types of cancer usually look like scaly patches or pink bumps on the skin that fail to heal. They can become scabby and bleed and are occasionally tender to touch.
Non-melanoma skin cancers can develop on any part of the body, but are usually seen on sun-exposed sites such as the face, neck, forearms and hands. In men, they can develop on the scalp, especially if there is little hair to provide protection.
They are the result of chronic sun damage over the years and usually affect people in their fifties onwards. However, you can see them in younger individuals, particularly if there has been a lot of sun exposure. These types of cancer have a much lower likelihood of spread compared to melanoma, and treatment is usually curative, often with surgery.
If a patient has noticed a non-healing patch of skin that fails to settle after a few weeks, it is worthwhile seeing their GP for evaluation to exclude these types of cancer. If there is a concern, they will be referred to a dermatologist.
Sun protection is the single most effective method for reducing the risk of skin cancer. This is particularly important if they have risk factors such as fair skin, family history or many moles.
Cover up This remains the first-line option in protecting against the sun. This should be something people think about on a hot, sunny day in the UK, whilst on a tropical holiday or even when participating in outdoor sport. Clothing, hats and sunglasses all have a role to play.
Shelter Ideally, try and stay out of the sun during peak daylight hours, when the sun is most likely to cause burning. This is usually between 11 a.m. and 3 p.m. Try and seek shade during these times.
Sunscreen
Look for a broad-spectrum sunscreen that offers protection against both UVA and UVB rays from the sun. This should be a minimum of SPF 15–30. Sunscreens can be of two kinds – mineral and chemical. Chemical sunscreens need to be applied for at least 20 minutes before going outdoors. Mineral sunscreens contain zinc and titanium and work as soon as they are applied. Sunscreens need to be reapplied every ninety minutes to get the stated protection factor on the bottle, and most of us are guilty of not reapplying it as frequently as we should. Also, remember to reapply after swimming and sweating. It is best to avoid once-daily formulations, as they are not likely to be as effective. Most of us also do not use the correct quantities of sunscreen for it to be effective. Sunscreen needs to be used on all areas not covered by clothing. About one shot-glass full (or 35ml) should be about right for an averagesized adult. A rough rule of thumb is about a teaspoon per body area: one teaspoon for the face, head and neck, one for each arm, one for each leg, one for the chest and abdomen and one for the back and the back of the neck. Remind patients not to forget their ears and the tops of their feet; these are commonly missed sites.
Many people do not use sunscreen on cloudy days. This is, in fact, the time we often see the worst sunburn due to false security that there is no sunshine around. We still need sunscreen on cloudy days.
I often get asked if it is necessary to wear sunscreen every day, including during the winter months. It is true that there is less UVB radiation in the winter in the UK, the main ray that can cause burning. However, as many skin cancers develop due to cumulative UV exposure, it is worthwhile getting into the habit of wearing sunscreen on exposed sites daily. For those who are concerned, it will also have benefits for the skin from an antiageing perspective.
Special care needs to be taken with small children in the sun. Blistering sunburn in childhood can double a person’s risk of developing melanoma in later life. Young skin is particularly vulnerable to the effects of ultraviolet radiation. Babies below the age of six months have little melanin in their skin, and their skin is too sensitive for the use of sunscreens. It is therefore important that young babies are not left in direct sunlight. After six months of age, sunscreen is safe to apply.

A case of nodular basal cell carcinoma

A case of an invasive squamous cell carcinoma.
DR ANJALI MAHTO
Dr Anjali Mahto is a highly respected and renowned medical and cosmetic consultant dermatologist and the author of the best-selling book The Skincare Bible. Based at her London Clinic in Harley Street, Dr Anjali employs a bespoke and tailored approach for all of her patients and is renowned for her quality service and unrivalled patient care.