CLINICAL
SURGICAL MANAGEMENT OF CLEFT LIP WITH LIP AUGMENTATION
Miss Rumi Kisyova describes how cleft lip cases are managed through a combination of surgical reconstruction techniques
The surgical management of a cleft lip with lip augmentation can be complex, especially in adult patients. Primary lip repair is typically performed between three and six months of age. Techniques continue to improve; however, differences from the ideal still present such as contour asymmetry, volume deficiency, or lack of projection.
Once the underlying dental support is optimised, secondary cleft lip deformities are related to the skin and subcutaneous tissue or the underlying muscle. The residual deformity is also influenced by the type of cleft lip that has been repaired – an incomplete cleft involving the separation of the white roll and the vermilion border, or a complete cleft involving the full height of the lip and the nasal sill. Additionally, the lip can be unilateral or bilateral, requiring different surgical approaches.
CLASSIFICATION OF CLEFT LIP

Unilateral Incomplete
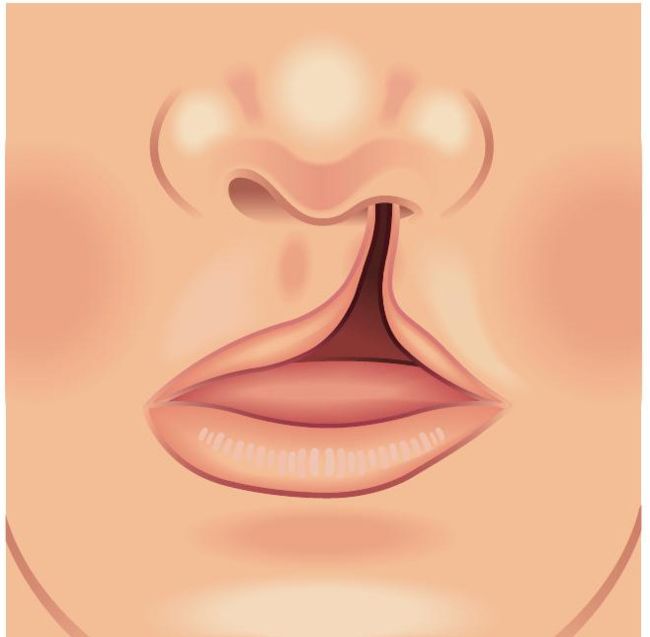
Unilateral Incomplete
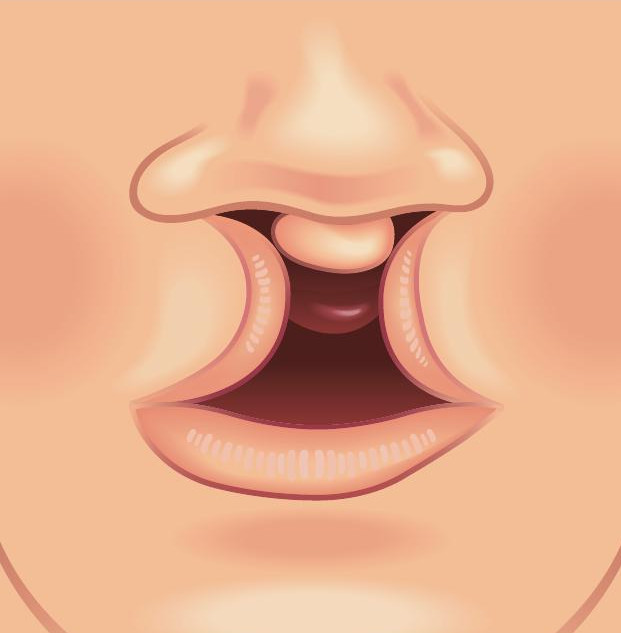
Bilateral Incomplete
In our practice, we have used a combination of surgical reconstruction techniques to restore lip projection, volume, and function, including dermal fillers, free fat grafting, and dermal fat grafts. Dermal fillers are a well-recognised option for managing cleft lips, especially for patients who prefer non-surgical intervention or want to preview their lip appearance before committing to a surgical procedure. Recent evidence supports the clinical finding that some regenerative effect may occur where dermal filler induces new deep tissue growth (such as calcium hydroxylapatite or poly-L-lactic acid fillers). We use dermal fillers to restore volume and lip contour, often combining the procedure with scar excision or a Z-plasty for improved results.
In cases where the patient has suboptimal results from the primary cleft lip repair combined with extensive scar tissue and volume or projection deficiency, using a dermal filler may accentuate the asymmetry as it may not be distributed evenly. Subcision of any tethered deep aspect of the cutaneous scar, particularly from the underlying orbicularis muscle may be undertaken before fat transfer. However, in cases where the intracutaneous aspect of the scar is the problem, micro fat grafting to the lip with or without scar revision may be a better option. The fat graft alone allows scar tissue to soften and expand, leading to better cosmetic results, particularly with repeated procedures. Typically, the procedure is performed under general anaesthesia, involving harvesting a small amount of fat from the inner knee. The harvested fat is then processed for micro fat graft implant and deposited in the lip using a fine cannula. As part of the consultation and consent process, the patients are warned that only a fraction of the micro fat graft will survive, and sometimes more than one procedure may be required.
A technique that has better longevity of results is the utilisation of a dermal fat graft, where a thin strip of dermis and fat is placed in the lip through a surgically created tunnel.1 This process addresses both the volume and the lip projection, as well as the lip contour. In our practice, we harvest the graft from the non-hairbearing area of the groin. The process involves marking a graft that corresponds to the length of the lip. Once the graft is marked, the epidermis is excised and the dermis with a thin layer of underlying fat is harvested. A tunnel is created in the lip using a fat-harvesting cannula, a process that has a dual action: tunnelling and breaking down the scar tissue. Once the graft is positioned at the desired location, the entry will be closed with resorbable sutures.
Volume and projection optimisation of the cleft lip can be a challenging process. Restoring the anatomical subunits as well as possible when performing the primary cleft lip repair is of essential importance and determines the potential secondary surgical interventions a patient may need. In our experience, a combination of techniques, such as the application of dermal fillers, micro fat graft, and dermal fat graft, can be used with excellent clinical results.
The article was cowritten with Mr Shaheel Chummun MBBS, MRCS, FRCS (Plast) MASurg (Cranio) consultant plastic and reconstructive surgeon and Mr Alistair RMCobb MBBS, BDS, FRCS (OMFS), FDSRCS (Eng), MFSEM (UK) clinical director and consultant surgeon, South West Cleft Service.
MISS RUMI KISYOVA
Miss Rumi Kisyova, MD, MSc (Lon), MRSC (Eng), is a plastic and reconstructive surgery doctor with a special interest in skin health and skin cancer prevention.
After graduating from Medical University Sofia, Bulgaria, Miss Kisyova completed a master’s degree in Clinical Neurosciences at King’s College, London. Over the last 12 years, Miss Kisyova has gained experience in various surgical subspecialties, allowing her to apply a holistic approach when treating her patients. While Miss Kisyova works as a full-time plastic surgeon in the NHS, she is also an aesthetic consultant passionate about helping her patients improve their skin health, wellness, and longevity. She is amember of the British Medical Association and the Royal College of Surgeons. Her co-authors on this article were consultant plastic and reconstructive surgeon Mr Shaheel Chummun MBBS, MRCS, FRCS (Plast) MASurg (Cranio) and South West Cleft Service clinical director and consultant surgeon Mr Alistair RMCobb MBBS, BDS, FRCS (OMFS), FDSRCS (Eng), MFSEM (UK).

REFERENCES
1. Surgical correction of upper lip deficit in patients with cleft lip using dermis fat graft Abdali H.
2. Current approaches to cleft lip revision
Garland K., Matic D. Current Opinion in Otolaryngology and Head and Neck Surgery 2019;27(4): 287-293.
3. Cleft Lip Nicholas J. Walker; Sachit Anand; Silvio Podda.
4. Use of Hyaluronic Acid Filler in Patients with Secondary Cleft Lip Deformity CMRivers
5. The usefulness of Microfat Grafting in Patients With Repaired Cleft Lip Yong Chan, B.; et al.