ROSACEA
Seeing red
Laser expert Kerry Belba breaks down the common subtypes of rosacea and explains how to treat them for the best patient outcomes
KERRY BELBA
Kerry Belba is a laser practitioner, trainer, key opinion leader and owner of Laser Skin Solutions in Bournemouth. She is the first aesthetic laser practitioner to have recently been voted onto the British Medical Laser Association (BMLA) board. Follow Kerry: @LaserskinsolutionsUK (Instagram) and @LaserSkinBournemouth (Facebook).
During my 16 years as a laser practitioner and clinic owner, I have seen my fair share of rosacea clients.
This progressive inflammatory vascular condition, usually affecting (but not limited to) white, northern European skin types, can often be the source of daily misery, anxiety and mental health issues for many people. The good news, however, is that laser and intense light sources (IPS), commonly known as intense pulsed light or IPL, can be extremely effective at managing this incurable disorder, giving clients or patients the relief they desperately crave.
WHAT IS ROSACEA?
Rosacea is a chronic vascular skin condition, usually affecting the face. It tends to present in lighter skin types and is characterised by facial flushing, redness, visible broken capillaries or thread veins, as well as red bumps or “spots” which are often confused with acne. In severe cases, rosacea is also sometimes mistaken for eczema or an allergic skin reaction. It is more common in women, but when affecting men the symptoms can be more severe. Rosacea mainly affects the nose, cheeks, chin and forehead, but can also cause inflammation and irritation of the eyes and eyelids, known as ocular rosacea. Although it is far more common in lighter skins, it can also affect people of colour. While it can often be hereditary, the pathophysiology of this condition is largely unknown.
Rosacea has four distinctive subtypes and knowing how to recognise these is essential to providing successful treatment plans for your clients. As a non-medical practitioner myself, it’s important to emphasise that as aesthetic laser practitioners we are not diagnosing skin disorders, but rather drawing on our education and training to recognise skin conditions as being either appropriate for laser/ IPL treatment, or in need of referral to a doctor or dermatologist. It’s essential that practitioners do not automatically assume that all rosacea types are suitable for laser or IPL as the first port of call. Knowing and recognising the rosacea subtypes is critical to your client or patient’s journey and their treatment plan.
ROSACEA SUBTYPES
There are four main subtypes of rosacea with a fifth type now being more commonly recognised and referred for treatment.
Erythematotelangiectatic rosacea

Erythematotelangiectatic rosacea. Client treated at Laser Skin Solutions Bournemouth with the Lynton Lumina IPL 585nm handpiece.
This very common subtype of rosacea presents with permanent erythema (redness) with a tendency to flush and blush easily. Usually small blood vessels are visible near the surface of the skin and are often accompanied with burning or itching sensations. Laser, IPL and LED are excellent treatment options for this subtype. My treatment approach is to clear as much of the vessels as possible using IPL, followed by a course of LED light therapy to address any residual redness.
It’s important to clarify that only lasers or IPLs will actually get rid of broken veins and capillaries by heating and coagulating the blood. White blood cells (macrophages) then clear up the dried blood in the same way that the body clears a bruise, a process called phagocytosis. While LEDs are not able to coagulate and clear broken vessels, powerful medical grade LEDs are excellent at vasoconstriction and reducing general redness. Topical creams prescribed by doctors can also provide short-term relief.

Papulopustular (inflammatory) rosacea
This equally common rosacea subtype can present with some, or quite substantial, permanent redness accompanied with red bumps (papules) with some pus filled (pustules) which typically last one to four days. This subtype is often confused with acne and historically was referred to as “acne-rosacea’”. It’s important to clarify that acne and rosacea are poles apart in terms of their pathology. While rosacea is a progressive inflammatory vascular disorder, acne on the other hand is a complication of the pilosebaceous unit in the skin. That’s not to say that someone with rosacea cannot also have acne, but the rosacea “spots” present in this subtype are very different to the commonly termed “whitehead”.
Interestingly, the common demodex mite, (D. folliculorum) naturally present in our skin, seems to go into reproduction overdrive in patients with papulopustular rosacea. The National Rosacea Society in the US estimates that rosacea patients have up to 18 times more D. folliculorum mites than patients without rosacea. It is not clear whether the mite itself is the cause of this very inflammatory subtype of rosacea, or whether the increased inflammation is in fact providing the perfect breeding ground for these mites to go into overdrive.
Papulopustular rosacea can be difficult to treat and treatment of this subtype should include a multi-faceted approach. It is essential that the inflammation is brought under control with medications or LED phototherapy before treating with laser or IPL. Antiinflammatory prescription treatment (topical or systemic) will help to reduce the inflammation and discomfort present. Soolantra (ivermectin) gets the demodex mite under control and also has anti-inflammatory properties.
If unsuccessful after three months, an antibiotic like Doxycycline can be prescribed for its anti-inflammatory effect. For a non-medicated approach LED light therapy can prove very effective at both reducing the inflammation in the skin and providing relief to the client. Patients can then be assessed on a case-by-case basis for Laser and/ or IPL but only once inflammation has subsided.

Papulopustular rosacea. Client treated at Laser Skin Solutions Bournemouth with a combination of the Lynton Lumina 585nm handpiece and Dermalux LED phototherapy.
Phymatous rosacea
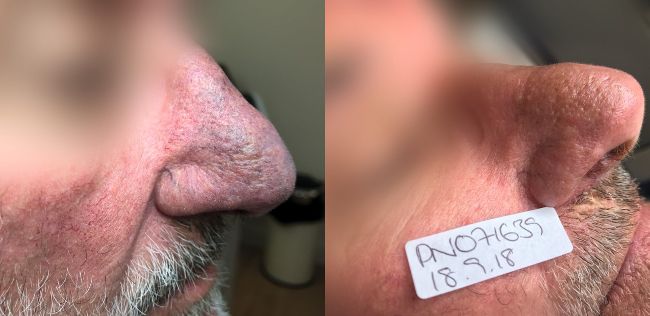
Phymatous rosacea. Client treated at Laser Skin Solutions Bournemouth with the Lynton Lumina IPL 585nm handpiece. Here you can clearly see the beginnings of rhinophyma where the skin on the nose has started to thicken. If the skin thickening were to continue to worsen, a CO2 resurfacing laser would be required for nasal tissue reconstruction.
This subtype is commonly associated with rhinophyma, a progressive skin condition causing the development of a large, bulbous nose. Sometimes referred to as a “drinker’s nose”, alcohol has in fact little to do with the pathology of phymatous rosacea (or indeed any form of rosacea), but can exacerbate the symptoms like flushing, redness, heat and discomfort. Other symptoms include thickening of the skin and irregular surface nodularities. Phymatous rosacea can affect the chin, forehead, cheeks, eyelids and ears.
Laser and/or IPL can be used in a bid to stop or slow the progression of phymato rosacea. Nasal reconstruction can also be achieved using an ablative CO2 laser.
Ocular rosacea
Ocular rosacea affects the eyes and eyelids, causing dryness and irritation. Some people report symptoms including foreign body sensations in the eyes, as well as itching and burning. Opthamologists can help manage this condition with, among other things, the use of steroid eye drops and Soolantra (ivermectin) cream for the skin on the eyelids. While laser or IPL cannot be performed on the face beyond the periorbital bone (without the use of intraocular eyeshields), it is quite common for ocular rosacea to improve when a client is having their nose and cheeks treated for the erythematotelangiectatic or phymatous subtype. Over the last 16 years, I have seen ocular rosacea drastically improve for clients, even though I have not treated them past the eye bone area. While the laser light is not applied beyond the eye bone itself, the heat nevertheless will continue to travel along the vessels and up to the eyelids, causing the heating and destruction of the offending vessels. This in turn reduces the inflammation on the lower eyelids, giving ocular rosacea clients some much-needed relief.
Neurogenic rosacea
Often mistaken for erythematotelangiectatic rosacea, this subtype presents with redness and intense stinging or burning sensation in the facial skin.
This complicated and poorly understood form of rosacea is multi-factoral, involving the nervous, vascular and immune systems in the body, as Dr Alia Ahmed, known as The Psychodermatologist, explains: “The receptors responsible for detecting pain, temperature and taste are known as transient receptor potential channels (TRP). People with rosacea have an increased number of some of these TRPs in their body. This results in hyper-reactivity or sensitivity to temperature change and flavour (e.g. spice) that may trigger symptoms of rosacea, as well as an increased likelihood to experience the itching or burning pain that is commonly reported by patients with neurogenic rosacea.
“Once activated, these channels release chemicals in the body that aggravate inflammation, as well as causing blood vessels to swell and become more open. This manifests as redness, swelling and flushing seen in rosacea, which can become a vicious cycle and cause persistent symptoms”.
Symptoms being reported by clients therefore will often be worse than what is being presented visually. As standard treatment approaches can be ineffective, it is advisable in the first instance to refer clients or patients back to their GP, as they may have neurological or psychiatric comorbidities which may benefit from a mental health referral. This is not to say however, that it is not possible or advisable to treat with laser or IPL.”
“Laser and IPL can be extremely effective at managing this incurable disorder, giving clients or patients the relief they desperately crave”
Shortly before lockdown, my first neurogenic rosacea client walked through my clinic doors. As is often the case, she was already under the care of a specialist, who had suggested she try laser treatment for her facial telangiectasia. This multifaceted approach involving dermatologists, pyschotherapists and laser practitioners lends itself to the best possible treatment outcomes for people with this rare rosacea subtype. Equally important in this multifaceted approach is the input of the client or patient themselves. The better their understanding of their condition and how it manifests for them, the better the treatment outcomes.
From a practitioner point of view, it is essential to continually update your rosacea knowledge and advances in understanding of this complex skin condition, by following organisations like Rosacea.org and becoming members of bodies like the British Medical Laser Association (BMLA); a unique platform for the exchange of knowledge, ideas, recent advances, and everything else in the field of lasers and light-based devices. This fantastic organisation is for all medics, surgeons, nurses, technicians, aestheticians and scientists who are directly or indirectly involved in the use of such devices for improving their patients’ and clients’ health and wellbeing. This year, the nurse’s and therapist’s session at the BMLA Virtual Conference (taking place from 6 to 7 May) will have a talk specifically on rosacea.
In summary, combining your own continual professional development as a laser practitioner, and taking a holistic approach with your clients, helping them to establish what their flare-up triggers are, not only empowers them to manage their own condition, but provides the best chances of daily relief, from this lifelong skin disorder.