CLINICAL
In orbit
Cosmetic eye treatment expert Dr Uche Aniagwu explains the optimal way to assess the infraorbital region before using fillers
DR UCHE ANIAGWU
Dr Uche Aniagwu MBBS MSc BSc is a leading non-surgical under-eye rejuvenation practitioner. He is a resident injector at Beyond Medispa at Harvey Nichols in London and is founder of The Cosmetic Eye Clinic and founder and clinical lead of the Under Eye Masterclass Training Programme.
As healthcare professionals in the field of aesthetics, we often find ourselves catering to the changing needs and concerns of our patients. So, when emerging insight signalled a rise in patient concern around the infraorbital region, I found myself intrigued. In one study of women over 30, 50% were found to be concerned about the appearance of their under eyes.1 A second study with 603 respondents found that tear troughs were the second largest concern after crow’s feet in women aged 30-35. Women aged 60-65 have also cited the infraorbital region as their third highest overall concern, behind crow’s feet and oral commissures.
But despite its growing priority among patients, the infraorbital region is only the seventh most-corrected area1 when accounting for all aesthetic treatments on the face. It is possible that some of this treatment gap is due to misconceptions about the danger of infraorbital treatments and general fear surrounding such procedures. I personally believe, however, that a far more likely cause is patient exclusion; in other words, practitioners schooled in older training methods do not see these patients as viable candidates for the non-surgical treatments with which they are familiar. And while I agree that the surgical versus non-surgical decision line is quite fine for the periorbital region, my experience also suggests that, by modernising our assessment training, practitioners would be able to confidently manage a far wider array of patients than current standards advise.
In addition to an expanded patient pool, the ability to conduct a modern, comprehensive infraorbital assessment provides a number of benefits to aesthetic practitioners: reduced complication rates, improved treatment results and greater confidence in declaring a patient more suitable for surgery. Sadly, this treatment area places too little emphasis on the assessment stage, resulting in practices that are outdated and poorly optimised. But conducting a comprehensive infraorbital assessment is actually very straightforward, and by overhauling our practices, we practitioners can potentially double the number of patients treated confidently and safely with hyaluronic acid filler.
Now, let’s have a look through the key assessment steps.

Puffy eyes before and after. Image: Dr Uche. Patient permission to share.
HISTORY
Firstly, it’s helpful to note that most infraorbital complaints fall into one of the following four categories: bags, sunken, wrinkles/ grooves or dark circles. Elementary as this point may seem, a patient’s history can actually tell the thorough practitioner quite a lot and offer immediate insights about viability. I often find a comprehensive overview of patient history to be the most critical step in filtering out unviable patients, doing so more efficiently than observation in many cases. In fact, I would recommend that any patient assessment begin with establishing a narrative around their lifestyle; do they get enough sleep? Do their eye bags have a diurnal pattern of fluctuation? Are they vegetarian or vegan and therefore possibly anaemic? After all, our role as practitioners is to help patients achieve a desired outcome, which doesn’t always require sticking needles in them. So, if a lifestyle alteration is likely to bring our patients closer to that desired outcome, we should make that recommendation before proceeding any further.

Wrinkled eyes. Image: Dr Uche. Patient permission to share.

Sunken eyes. Image: Dr Uche. Patient permission to share.
PATIENT POSITIONING
Far too often when I see practitioners performing assessments on a treatment bed or chair, their patient is lying back at a 45-degree angle (or greater in some cases). But optimal observation occurs with the patient as upright as possible; a position which allows gravity to act on the face naturally, and is thus the best way to assess and plan. Sometimes lying the patient back can also cause the nasojugal fat pad, under which the angular artery runs, to spread over the tear trough groove and give the face an artificially even appearance. Additionally, ensure that you have good lighting wherever you choose to position the patient. A good amount of natural light is often sufficient, but if using artificial light, I’d recommend fluorescent white light directly in front of or above the patient.
“Contrary to conventional belief, treating the infraorbital area is safer than procedures on laughter lines”

Patient assessment with a slightly negative vector. Image: Dr Uche. Patient permission to share.
UNDERSTANDING VECTORS
Vector assessment, or the lack thereof, is another shortcoming of conventional training, and one which often causes practitioners to significantly favour treatment of patients with sunken eyes over those with undereye bags. But by understanding the anatomy of the infraorbital region, how it evolves with ageing and the different ways vectors can guide your treatment plan, practitioners can properly assess and often treat patients with puffy eyes or bags.
Vectors, which refer to the frontal cheek projection in relation to the corneal line (the perpendicular line that sits in front of the cornea), are split into positive, negative and neutral. If you’ve ever heard that treating the cheeks can improve the condition of eye complaints, vectors are the key. As the face ages, the frontal cheek volume declines and recedes. Infraorbital fat very often begins to prolapse and sit forward relative to the cheeks. This phenomenon, also known as a negative vector, gives the appearance of pronounced eye bags. By adding volume to the cheeks and doing some careful work along the tear trough ligament, a practitioner can restore a patient’s youthful, positive vector and significantly improve the appearance of eye bags. For patients with negative and, in some cases, neutral vectors, this simple assessment, which requires only a tablet or smartphone image, can provide an additional treatment option and give practitioners confidence in managing far more patients. Furthermore, this same technique can be used as a strong indicator to avoid those with bags under the eyes who still have a positive vector.
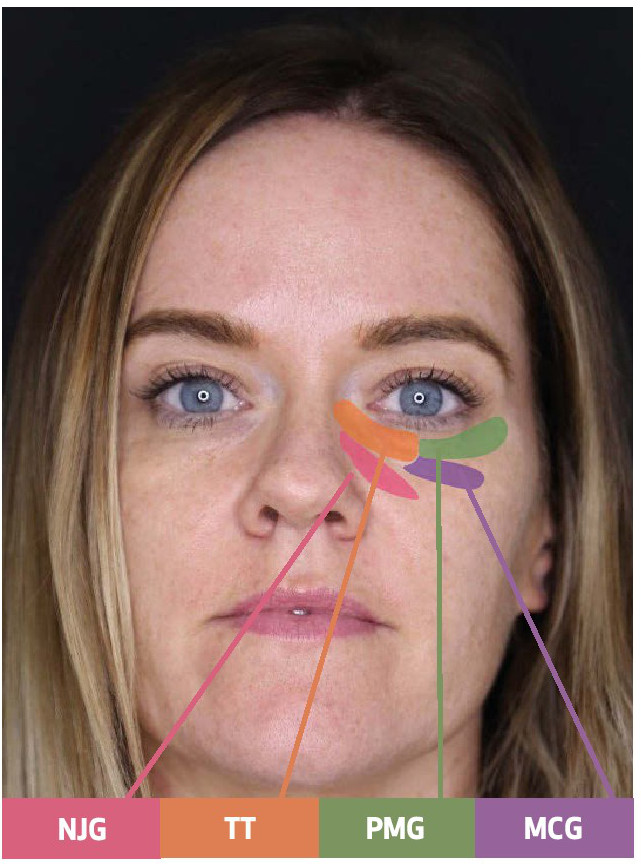
Surface anatomy. NJG: Nasojugal groove, TT: Tear trough, PMG: Palpebromalar groove, MCG: midcheek groove. Image: Dr Uche. Patient permission to share.
SKIN QUALITY
Assessing skin quality is another important procedural step for practitioners looking to improve success rates. Regardless of the findings from a patient history and lifestyle assessment, I recommend that practitioners look out for two specific conditions with regards to the skin. First is hyperpigmentation; no amount of deepto-bone hyaluronic acid fillers will improve the appearance of hyperpigmentation. You can get a feel for the extent of the hyperpigmentation by stretching the skin and observing how much, if at all, the colouring fades. If minimal fading occurs, signalling that the patient has significant hyperpigmentation, a practitioner should avoid treating as normal. Rather, you should consider topical treatment or even mesotherapy with other hyaluronic acid products, which have been shown to improve hyperpigmentation.
Secondly, any practitioner should consider a patient’s skin laxity, particularly in older patients, as a factor in deciding whether or not to treat. Not only can loose skin pose a real challenge when assessing your work, but it also frequently presents an obstacle to patient satisfaction with the procedure. One method that I like to use in assessing a patient’s infraorbital skin laxity is the “snap test” – stretch the skin downwards and hold for two seconds, release and observe the recoil. If the recoil takes longer than two seconds, skin elasticity is suboptimal, and I would consider the skin to be lax. Properly accounting for lax skin requires a very advanced practitioner, and I would suggest avoiding treatment under such circumstances.
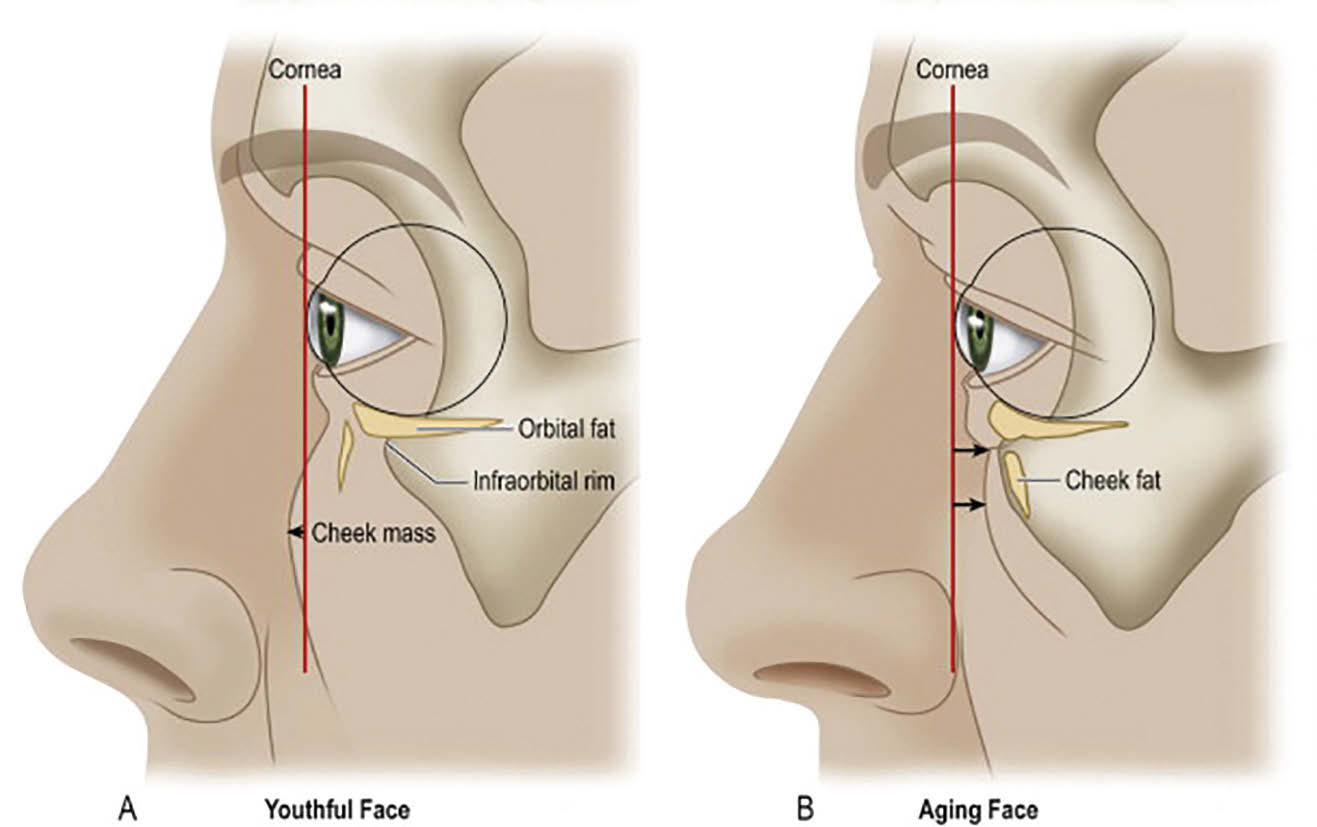
The first image demonstrates a positive vector with the cheek mass in front of the corneal line and the infraorbital fat further back. The second image shows a negative vector where the cheek mass sits behind the corneal line and the infraorbital fat is further forward.4
CONCLUSION
As aesthetic practitioners, we have a responsibility to understand patient needs and offer the best possible solutions, which may or may not include filler treatment. Yet, recent research shows a clear gap between the priority of patients’ infraorbital concerns and the frequency with which practitioners treat such issues – a gap that I believe can be addressed, in large part, by modernising our industry assessment practices. By combining a thorough patient history with some very simple, revealing assessment tools, practitioners will be able to make far better-informed decisions as to whom they do and do not treat. More information will lead to greater confidence in treating a wider range of patients, not just the eye hollows to which we’ve become accustomed.
Furthermore, by doing our due diligence in applied anatomy and assessment, we practitioners can expect improved treatment results and patient satisfaction, both of which are robust barometers of success. Contrary to conventional belief, treating the infraorbital area is safer than procedures on laughter lines, noses or temples, and lags far behind in potential for filler-induced blindness or other complications. So, with these common misconceptions dispelled, the primary obstacle that remains is confidence, which can be boosted significantly by completion of a thorough, contemporary assessment.
References
1. Arcane Research Study – February 2011: study carried out in France among 4 402 women aged 18 to 75.
2. Narurkar, V., Shamban, A., Sissins, P., Stonehouse, A., Gallagher, C. Facial treatment preferences in aesthetically aware women. Dermatol Surg. 2015,41 Suppl 1:S153-60.
3. Teoxane Redensity II brochure, July 2016: *Results based on opinion from n=603 patients aged from 30-65 years old
4. Pessa et al. (Aesthetic Plast Surg. 23:337, 1999.)
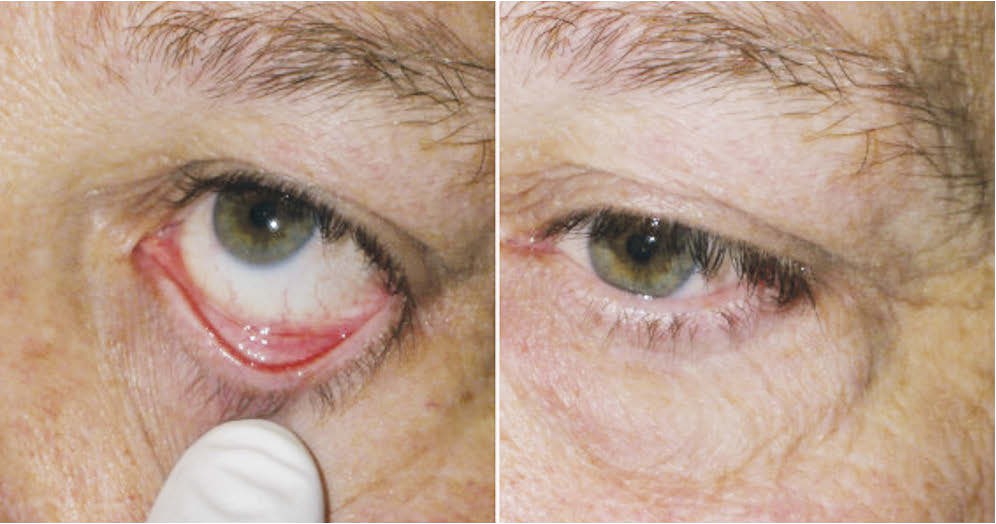
Image of “snap test” being performed. Image: plasticsurgerykey.com